The Blood-Brain Barrier: A Defensive Line Still Missing its Star Player, Neuroprotection
Executive Summary
- Drug delivery vs. neuroprotection:
The pharmaceutical industry has heavily invested in blood brain barrier (BBB)-crossing technologies (e.g., Roche’s Brainshuttle™, GSK’s Grabody-B, and intranasal agents such as SPRAVATO), but far less in therapies that maintain or restore barrier integrity. - Neuroprotective approaches:
Strategies currently under evaluation include modulation of endothelial cell transporters, upregulation of tight junction proteins (e.g., claudins and occludins), suppression of neuroinflammatory pathways, exogenously supplying extracellular matrix-derived biopolymers to rescue gaps in the endothelium triggered by the loss of tight junctions, and transplantation of neurovascular-supporting cells such as pericytes. - Challenges:
Failures such as natalizumab’s (TYSABRI) inability to reduce seizure frequency in drug-resistant focal epilepsy underscore the heterogeneity of BBB-related pathology and the need for tailored therapeutic approaches; natalizumab targets the BBB’s α4-integrin-VCAM-1 interaction, a pathway central to multiple sclerosis etiology, but likely less relevant in epilepsy. - Outlook:
Approximately ten companies are currently exploring neuroprotective candidates across various indications. However, most programs have remained in early- to mid-stage development for an extended period. Accelerating progress by strategically shifting gears in the discovery and development process is therefore of paramount importance: BBB-targeted neuroprotection could be a paradigm-shifting, billion-dollar opportunity, reframing the BBB from an obstacle to a frontline therapeutic target in some disease areas. Success will depend on mapping actionable targets, advancing biomarkers/imaging, and aligning interventions with disease-specific mechanisms.
The blood-brain barrier (BBB) plays a central role in the pathophysiology of many neurologic diseases, acting as both a physical and functional shield regulating the movement of substances between the bloodstream and the brain. As research uncovers the intricate mechanisms underlying BBB dysfunction, ranging from impaired endothelial tight junctions and disturbed neurovascular unit signaling to pro-inflammatory cytokine activation, the concept of neuroprotective treatments targeting BBB components has been gaining attention, although not enough. Promising strategies include modulation of endothelial cell transporters, upregulation of tight junction proteins (such as claudins and occludins), suppression of neuroinflammatory pathways, exogenous supply of extracellular matrix-derived biopolymers to rescue gaps in the endothelium triggered by loss of tight junctions, and transplantation of neurovascular-supporting cells like pericytes. Ultimately, therapies able to restore or stabilize BBB integrity may not only prevent neuronal injury but also offer disease-modifying potential in disorders characterized by BBB dysfunction, such as stroke, epilepsy, neurodegenerative diseases, and brain cancers. However, mapping which BBB targets are actionable and how to personalize interventions for specific disease contexts remains a critical focus for the future of neuroprotective medicine.
The BBB can be likened to a defensive line in American football, standing guard to protect the brain from harmful substances while regulating what enters from the bloodstream. In this analogy, just as a strong and coordinated defense prevents the opposing team from advancing and scoring, a robust BBB shields neural tissue from damage and inflammation. However, when the BBB is compromised, a situation similar to a weak defensive line letting through key plays, neuronal injury and disease progression can ensue. Understanding and targeting the unique mechanisms that maintain BBB integrity in each disease is essential to developing neuroprotective therapies that effectively "strengthen the defense" and modify disease outcomes across neurological disorders.
Unmet Needs in BBB Research:
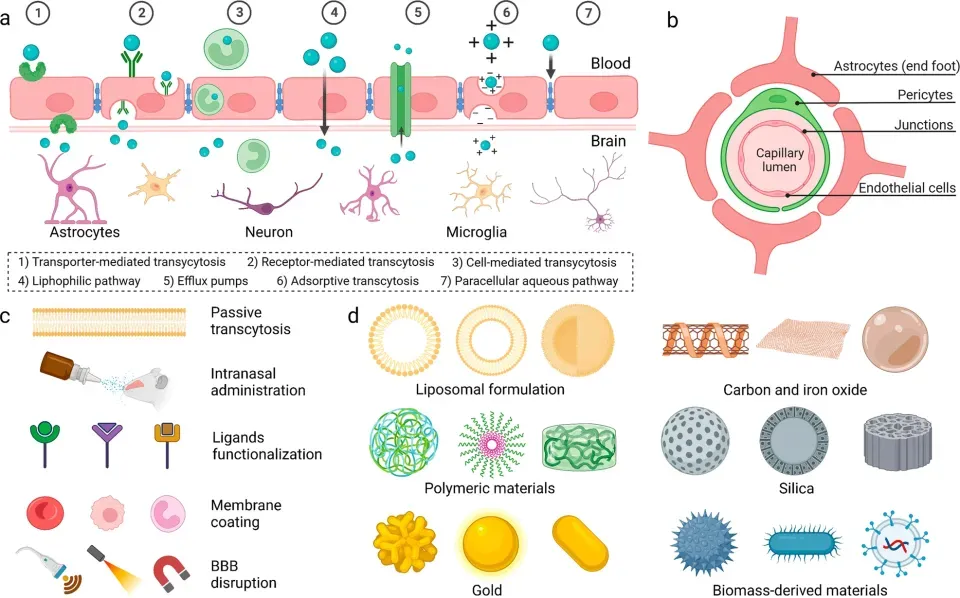
Given the crucial role the BBB plays in safeguarding the brain, extensive drug delivery research has been aimed at crossing it. Methods of drug delivery across the BBB are being heavily investigated, including the use of membrane coating (e.g., Lu et al., J Control Release 2017) and nanocarriers (e.g., Parbhu et al., Nanoscale 2017). Some approved therapies utilize intranasal administration for rapid brain delivery, such as SPRAVATO for the treatment of major depressive disorder. In recent years, pharma giants, such as Roche, BMS, AbbVie, Eli Lilly, GSK and others, have been working on brain shuttle technologies in neurological/ neuroinflammatory conditions. These technologies primarily rely on the use of engineered antibody-based vehicles that bind to targets on the BBB, which internalize them, along with the drug, into the brain. Among the most notable is GSK’s recently initiated collaboration to develop the Grabody-B platform using bispecific antibodies targeting the insulin-like growth factor 1 receptor to shuttle drugs across the BBB, as well as Roche’s Trontinemab - a bispecific antibody that combines the anti-amyloid-beta monoclonal antibody gantenerumab with a transferrin receptor 1 (TfR1)-directed Brainshuttle™ module, currently being evaluated in Alzheimer’s disease. These new technologies have the potential to revolutionize drug delivery aimed at crossing the BBB.
However, while extensive research has been done on crossing the BBB, a large unmet need remains for ensuring BBB maintenance, offering the ever-elusive neuroprotection. The BBB is crucial for the homeostasis required for neuronal functions, defending the system against toxic insults, regulating the communication between the periphery and the CNS, and providing the brain with nutrients. When this crucial barrier is compromised by physical or physiological forces it allows a flood of peripheral mediators, such as serum proteins, reactive oxygen species, and fibrin, to enter the brain. This breach can have devastating effects, leading to both immediate (e.g., neuronal injury, vascular damage, edema, or hypoxia) and long-term (e.g., post-stroke epilepsy, cognitive decline) consequences. Protecting the barrier from leaking may help stop, and even prevent, these from happening.
For over a decade, academic research focused on exploration of drugs that may potentially fortify the BBB. It begs the question, does neuroprotection have the potential to become a central endeavor in industry? Consider the potential: a billion-dollar game-changer. For example, take the countless micro-concussions an American football player endures over a career - long-term damage is almost certainly linked to the repeated opening of the BBB. Now imagine if we could provide these athletes with a "linebacker” to protect their brains from these harmful “offensive tackles”. Wouldn’t that be revolutionary?
Physiological state:
Before we delve into the pathologies, a quick introduction to the BBB. The human brain is supplied by ~400 miles of blood vessels that deliver oxygen and nutrients while clearing metabolic waste. Brain capillaries, providing nearly 12 m² of endothelial surface area, form a key component of the BBB. This barrier consists of specialized endothelial cells surrounded by pericytes, smooth muscle cells, and astrocytic end-feet. Tight junctions between these cells restrict the passage of blood-borne molecules, thereby maintaining a tightly regulated microenvironment enriched with brain-specific growth factors and signaling molecules. This protected milieu is immune privileged and essential for proper synaptic, neuronal, and network function. However, the BBB also is also the key reason for why many drugs do not reach therapeutic concentration in the brain, as they are excluded from it by the barrier.
Fig 1: Strategies and materials for BBB regulation and brain-targeted drug delivery. A) Schematic diagram of different mechanisms for BBB crossing. B) Schematic diagram of BBB structure. C) Engineered materials for brain-targeted drug delivery. D) Various non-invasive strategies for BBB crossing. Adapted from: Wu et al., Signal Transduction and Targeted Therapy volume 8, Article number: 217 (2023)
Pathological state:
The BBB is disrupted during various disease processes or physical insults to the brain, leading to a vicious cycle that causes a cascade of harmful events such as proinflammatory cytokine release, accentuating brain damage. Some of these can occur in cases of traumatic brain injury (TBI), epilepsy, stroke, and infection. Diseases such as Parkinson’s Disease (PD), Epilepsy, Alzheimer’s Disease (AD) and Multiple Sclerosis (MS) are also accompanied by changes to the BBB. However, it remains unclear what came first: the chicken or the egg – has BBB disruption caused these diseases, or is it an effect that happened later in the process of the respective disease?
Emerging research has begun to carve out a clearer chronological line between BBB dysfunction and most classes of neurological disorders (source), including post-stroke epilepsy. Stroke offers a good “case study” for this connection since the severity of stroke is directly linked to the extent of BBB damage, which is most evident in the infarct core, where the stroke occurs. This damage often coincides with serious post-stroke complications, such as post-stroke epilepsy. However, is there a causal relationship? A recent paper suggests that stroke-induced BBB dysfunction can trigger a cascade of events leading to either acute symptomatic seizures (≤7 days post-stroke) or unprovoked seizures (>7 days post-stroke). While this sequence begins to answer the “chicken or the egg” dilemma, the pathologic feedback loop epilepsy causes within the brain may trigger additional complications, such as strokes, creating an additional level of complexity. To tease apart the intricacy of this delicate balance, it is crucial to understand the factors playing a neural-protective role in BBB-maintenance.
Select therapeutic updates:
While the harm associated with BBB disruption is well studied, exploration of BBB maintenance-targeting drugs has been relatively scarce. Below, we outline some of that research, including the failures.
Among the more promising neuroprotective strategies for the BBB are blocking of the perivascular platelet-derived growth factor receptors, metabolic modulation of pericytes, directly targeting tight junction proteins, and integrating neurovascular-supporting cells like pericytes. Early-phase clinical trials evaluating agents such as imatinib (TKI) have shown reduced neurological disability in stroke patients by stabilizing BBB integrity, though causal links between preclinical benefit and clinical outcomes remain unclear. Conversely, targeted monoclonal antibodies (mAbs), such as natalizumab (TYSABRI; α4-integrin mAb) and enlimomab (ICAM-1 mAb), have failed to improve seizure or stroke outcomes, with enlimomab even worsening prognosis in ischemic stroke, highlighting the context-specific challenges of BBB interventions. Ongoing studies continue to explore novel molecular targets, such as claudin-3 and other tight junction proteins, and plans for future research include enhanced biomarker development/imaging modalities to optimize and personalize BBB repair strategies. The trajectory of BBB neuroprotective therapy will depend on translating mechanistic insights into safe, efficacious treatments tailored to the unique pathology of each disease state.
Positive results from potentially neuroprotective targets:
The oncology drug imatinib (GLEEVEC), a tyrosine kinase inhibitor, has demonstrated the ability to restore BBB integrity in pre-clinical studies and has shown promising results in reducing neurological disability in stroke patients. While a causal link has not yet been established between preclinical and clinical evidence, considering the additional pathways potentially underlying the clinical benefits, this, at the very least, warrants further investigation in stroke patients.
The angiotensin receptor blocker losartan (COZAAR), which is used as an anti-hypertensive and also known to inhibit TGFβ signaling, has been shown to reduce epileptogenesis in animal models. In humans, the angiotensin receptor blocker class was found to be significantly associated with a lower incidence of epilepsy compared to the other drug classes in patients with hypertension. TGFβ is a known modulator of the BBB and has been implicated in the development of post stroke epilepsy through stroke-induced BBB dysfunction. Although a direct link between losartan’s positive effects on epileptogenesis and BBB integrity has not yet been established, this connection merits further exploration.
Transplantation of iPSC-derived pericytes enhances BMEC interactions, upregulates the expression of tight junction proteins (multiprotein junctional complexes between epithelial cells of the BBB), and suppresses the expression of inflammatory markers (TNF-α and IL-1β), ultimately decreasing BBB permeability and conferring neuroprotection.
Studies targeting claudin-3 and other tight junction proteins highlight a rapidly advancing area in BBB therapeutics. Claudins, particularly claudin-1, claudin-3, and claudin-5, are central to BBB integrity, with upregulation helping to stabilize and restore barrier function in disease states such as metastatic brain cancer and neuroinflammatory conditions. Recent preclinical models show that manipulating claudin expression can both reduce BBB permeability during inflammation and prevent tumor cell invasion of brain tissue. For instance, RepSox, a claudin-5 modulator, has been shown to inhibit seizure activity in a kainic acid-induced mouse model of epilepsy. Additionally, there is growing interest in using tight junction protein profiling for companion biomarker strategies.
More recently, in an Alzheimer’s Disease mouse model, researchers demonstrated that nanoparticles targeting the low-density lipoprotein receptor-related protein 1 (LRP1) on the BBB significantly reduced brain Aβ levels by nearly 45%. Furthermore, cognitive assessments performed up to 6 months post-treatment revealed that treated AD mice exhibited significant improvements in spatial learning and memory, with performance levels comparable to those of wild-type mice. Per the researchers, the supramolecular drugs developed in this study function as a molecular “reset switch.” By mimicking LRP1 ligands, they bind to Aβ, cross the BBB, and trigger the clearance of toxic species from the brain. In doing so, they help restore the vasculature’s natural waste-removal function and return it to a healthy state.
In summary, the future of neuroprotective BBB research will likely center on exploiting the regulatory mechanisms to improve neuroprotection and CNS drug delivery, with outstanding questions including how molecular pathways are linked to clinical outcomes, how BBB-modifying interventions can be safely and selectively delivered, and whether restoring or stabilizing BBB integrity will translate into disease-modifying benefits across diverse neurological indications.
Negative results from potentially neuroprotective targets:
While the concept of targeting the neuroprotective features of the BBB holds exciting potential, it is important to recognize that this approach is unlikely to be a “one size fits all” solution. Each breach of the BBB whether from trauma, disease, or infection, presents its own complexities, making a universal treatment approach challenging. Instead, a tailored strategy may be needed to address the unique circumstances surrounding each disruption.
For example, commentary on the failed attempt to use natalizumab (TYSABRI; α4-integrin mAb) to reduce seizure frequency in patients with drug-resistant focal epilepsy highlights the variability of underlying pathology related to BBB disruption. Natalizumab disrupts the interaction between the leukocytic α4-integrin and the BBB molecule VCAM-1, which is upregulated during neuroinflammation and expressed on endothelial cells. While reasons for the observed outcome remain unclear, one hypothesis is that this interaction is likely more integral to the pathophysiology of multiple sclerosis than it is for epilepsy.
Certain mAbs, such as enlimomab, block ICAM-1 (a central BBB molecule) on the endothelium, preventing adhesion of white blood cells to the vessel wall. Because anti-ICAM antibodies appear to block an early step in reperfusion-related injury, they presented a hopeful mechanism for preserving neuronal function after stroke. However, it was found that not only was enlimomab not an effective treatment for ischemic stroke in the model studied, but it may also significantly worsen stroke outcome. Enlimomab’s failure implies that ICAM-1 may not be a viable target post stroke. Instead, other strategies should be explored such as tight junction protein modulation e.g., modulation of claudin-3, which has been shown to contribute to the expression and localization of other tight junction proteins, and contributes to the structure and function of the neurovascular unit (NVU).
Pepinemab (VX15/2503) is a humanized IgG4 monoclonal antibody developed by Vaccinex Inc., targeting semaphorin 4D to preserve glial and immune cell homeostasis. While its Ph2 Huntington’s disease trial did not meet its co-primary endpoints, Pepinemab demonstrated significant improvement in motor function versus placebo. The completed Ph1b/2 SIGNAL-AD trial further evaluated its safety and impact on brain metabolic activity over eight months. Results are yet to be published.
Failures to use the BBB as a treatment target largely stem from the inherent complexity and heterogeneity of BBB disruption across different diseases, injuries, and inflammatory states—making a “one size fits all” strategy impractical and sometimes counterproductive. For example, the unsuccessful use of natalizumab in drug-resistant focal epilepsy, despite its efficacy in multiple sclerosis, underscores how molecular pathways like the α4-integrin/VCAM-1 axis may not be equally relevant across neurological disorders. Similarly, the anti-ICAM-1 antibody enlimomab, though designed to reduce inflammatory injury post-stroke, failed clinically and even worsened outcomes, casting doubt on ICAM-1’s suitability as a target in this context. These examples highlight that BBB-targeted interventions can have variable or adverse effects depending on the underlying pathology, cell type specificity, and stage of disease. Outstanding questions remain about which BBB components are actionable to offer neuroprotection in given clinical settings, how to modulate them without unintended neuroinflammatory or neurotoxic sequelae, and what biomarker or imaging tools can guide safe, precision-targeted therapies.
The future of BBB research - Neuroprotection
An increasing number of companies are focusing on neuroprotection – including Athira Pharma, Accure, Nyrada, and Sanofi , with some even leveraging the BBB as a target. So far, >10 therapeutic agents have been identified, and are being developed by ~10 active biotechnology and pharmaceuticals companies to restore brain barriers integrity in neurodegenerative diseases and CNS injuries (Figure 2). The majority of these assets are in Ph1 - Ph2, with one marketed product, Biogen’s TYSBARI, currently serving as the standard of care for reducing immune cell migration across the BBB in patients with Relapsing-Remitting Multiple Sclerosis. A few examples of ongoing efforts to develop these assets are provided below. For a comprehensive and detailed review of the development landscape in the space, refer to Lemarchant, et al. Fluids and Barriers of the CNS. 22: 72 (July 2025).
Axoltis is developing NX210c – a 12-amino acid peptide analogue of the most conserved sequence of type 1 thrombospondin repeats, and promotes neuroprotection against glutamate-induced excitotoxicity. It has been granted orphan-drug designation by the FDA and the EMA for treatment of Amyotrophic lateral sclerosis (ALS). Among others, NX210c acts by tightening the BBB, and thus shows promise in a wide range of neurological indications. The asset is currently being evaluated in a Ph2 in ALS patients, with results expected in Q2 2026.
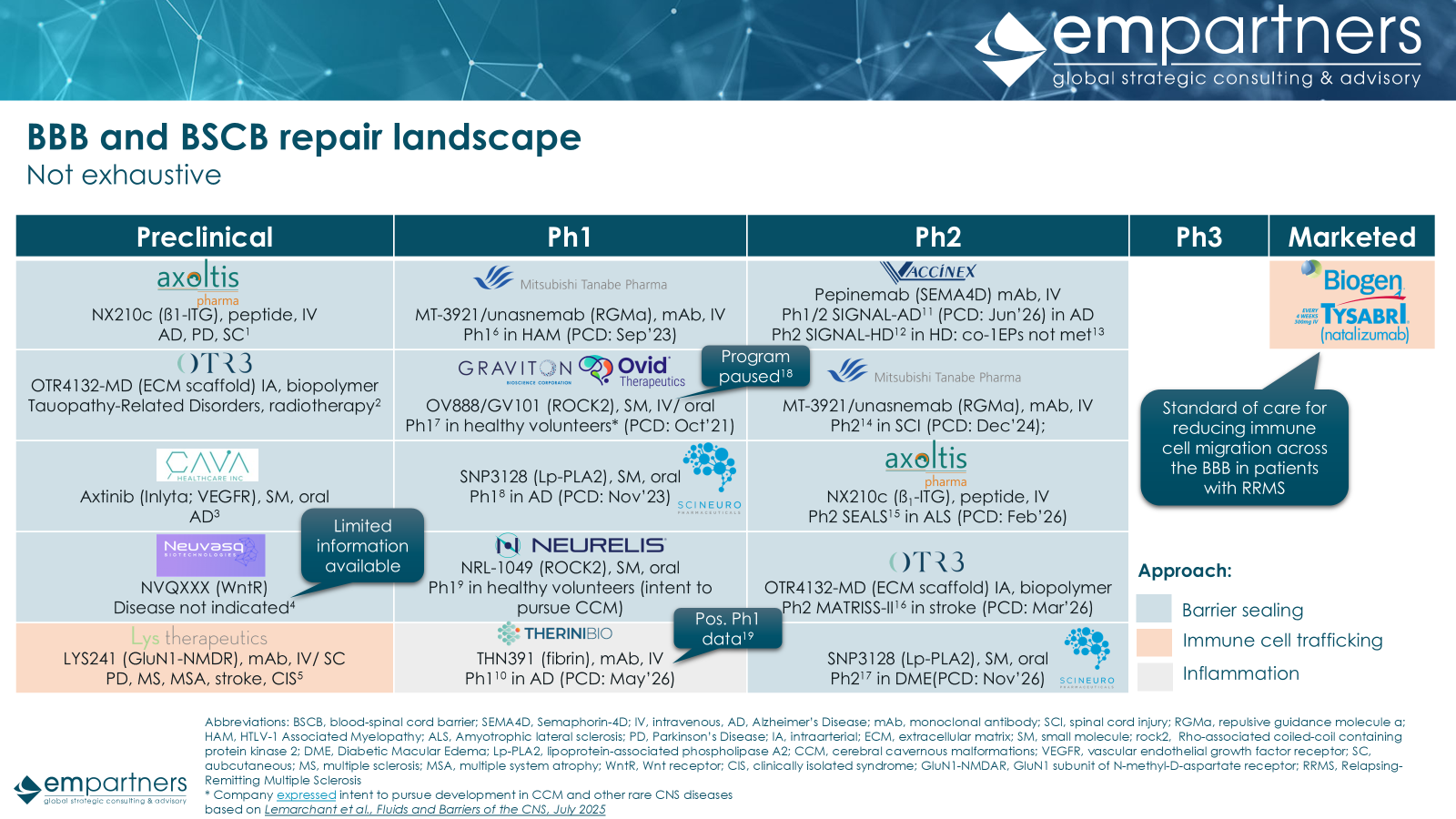
Figure 2: BBB and blood-spinal cord barrier (BSCB) repair landscape (not exhaustive, industry only)
Abbreviations: BSCB, blood-spinal cord barrier; SEMA4D, Semaphorin-4D; IV, intravenous, AD, Alzheimer’s Disease; mAb, monoclonal antibody; SCI, spinal cord injury; RGMa, repulsive guidance molecule a; HAM, HTLV-1 Associated Myelopathy; ALS, Amyotrophic lateral sclerosis; PD, Parkinson’s Disease; IA, intraarterial; ECM, extracellular matrix; SM, small molecule; rock2, Rho-associated coiled-coil containing protein kinase 2; DME, Diabetic Macular Edema; Lp-PLA2, lipoprotein-associated phospholipase A2; CCM, cerebral cavernous malformations; VEGFR, vascular endothelial growth factor receptor; SC, subcutaneous; MS, multiple sclerosis; MSA, multiple system atrophy; WntR, Wnt receptor; CIS, clinically isolated syndrome; GluN1-NMDAR, GluN1 subunit of N-methyl-D-aspartate receptor; RRMS, Relapsing-Remitting Multiple Sclerosis
* Company expressed intent to pursue development in CCM and other rare CNS diseases
See below for list of references.
Another interesting candidate is MT3921 (unasnemab), a humanized IgG1 mAb developed by Mitsubishi Tanabe Pharma targeting RGMa, a protein that inhibits neurite growth and disrupts endothelial barrier integrity. A Ph1 trial in TLV-1-Associated Myelopathy completed in December 2023 and confirmed safety and pharmacokinetics (PK). A Ph2 trial in acute cervical spinal cord injury completed in April 2025 evaluated efficacy on upper extremity motor function, with results likely expected soon.
OTR4132 (HSm4131) is a synthetic polysaccharide developed by OTR3 to mimic heparan sulfate’s neuroprotective functions, while resisting degradation. Following a Ph1 trial in ischemic stroke which confirmed safety, a Ph2 study is assessing OTR4132’s efficacy in acute ischemic stroke, and is expected to complete in March 2026. Following the success in Ph1, OV888 (formerly GV101) is a highly selective small-molecule ROCK2 inhibitor (hypothesized to restore endothelial barrier integrity and reduce fibrosis) developed by Ovid Therapeutics and Graviton BioScience for neurovascular diseases and cerebral cavernous malformation. However the program has been paused, per Ovid’s Q2 2025 investor report, in order to evaluate “clinical design learnings and regulatory feedback from recently completed competitor Phase 2 programs.”
In summary, much like the defensive line in American football stands as the first line of protection against an opposing offense, the BBB serves as a critical guardian defending neural tissue from potentially harmful substances circulating in the bloodstream. Effective neuroprotection hinges on fortifying this barrier, much like a strong, coordinated defense limits the opponent’s scoring opportunities. Targeting tight junction proteins, endothelial transporters, and even neuroinflammatory pathways to restore BBB integrity is akin to shoring up gaps in the defensive line, preventing breaches that could lead to neural injury. However, just as no single defensive strategy suits every opponent or game situation, BBB-targeted therapies must be tailored to specific diseases and injury mechanisms, necessitating precision interventions. Ultimately, optimizing BBB neuroprotection promises to shift treatment paradigms, transforming the BBB from a passive obstacle into an active therapeutic frontline against diverse neurological disorders.